Summary
Health professionals who care for patients with life-limiting conditions may adopt a palliative approach. This can prevent and relieve suffering and improve the quality of life for patients through good symptom control and support for them and their families.
This report covers health service use in the last year of life across multiple settings (hospital and community) and includes when care started and ended, and patient characteristics (such as sociodemographic and diagnoses). Within the baseline study population (136,000 'predictable deaths') of those aged 40+ who died in the 2019–20 financial year, two overlapping sub-populations were defined – those receiving specialist palliative care ('SPC', 52,000 individuals), and those in need of palliative care (109,000). The analyses assess individuals in all states except WA and NT using data in the period mid-2018 to mid-2020 contained in the Australian Institute of Health and Welfare’s (AIHW) National Integrated Health Services Information (NIHSI) linked data asset.
The population in need of palliative care captured 80% of all predictable deaths in 2019–20. In the last year of life, 2 in 5 (41%) of the population in need of palliative care received specialist palliative care (SPC) and 94% consulted with a GP; 1 in 2 (54%) had consultations with other specialists (Figure 1a).
Most SPC was received around 15 days before death. Current evidence suggests at least 3 to 4 months of specialist palliative care provides the maximum benefit.
The SPC population is younger than the population not receiving SPC.
There were 164,400 deaths between July 2019 and June 2020. To ensure accurate comparisons with the hospital data, deaths in WA and the NT were excluded (totalling 14,345 deaths).
Consultations with non-palliative care specialists were far more common for those receiving specialist palliative care than those not receiving specialist palliative care (68% vs 42%).
2 in 3 people dying from cancer received SPC. Cancer is responsible for 1 in 2 deaths in the SPC population, 3 times as high as in the population not receiving SPC.
Receipt of SPC is more common for those dying of renal or liver disease than for other non-cancer conditions.
On average, the likelihood of receiving SPC was greater for people living in major cities (compared to regional areas) and for those in socioeconomically advantaged areas (compared to disadvantaged).
For the population in need of palliative care, those dying of cancer were at least 5 times as likely to have Medicare-recorded consultations with palliative care specialist physicians than people dying from other causes (21% versus less than 4%).
Figure 1a: SPC service, cancer diagnosis and specialist consultations as proportions of the SPC population, compared with these as proportions of the population in need of palliative care
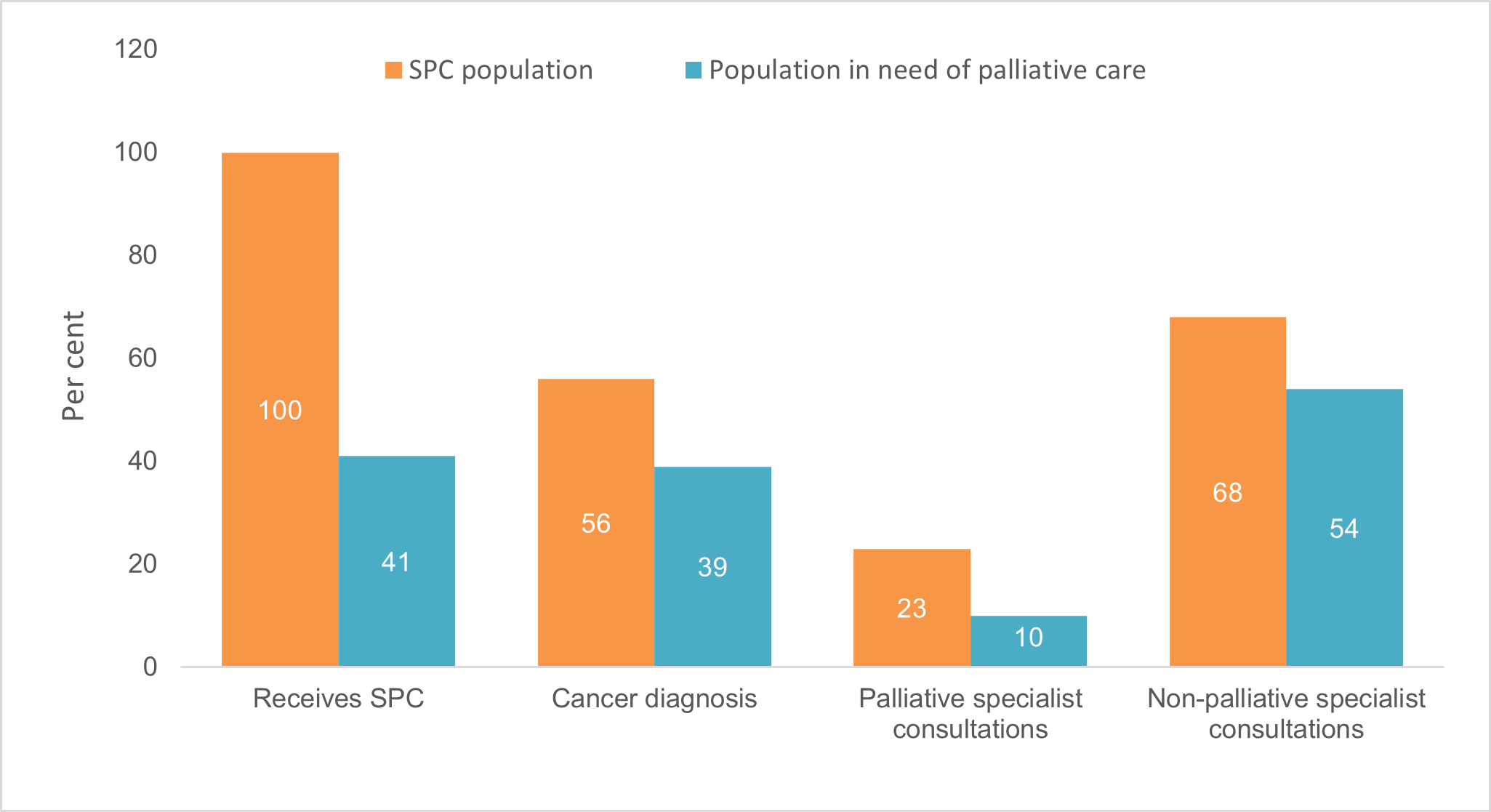
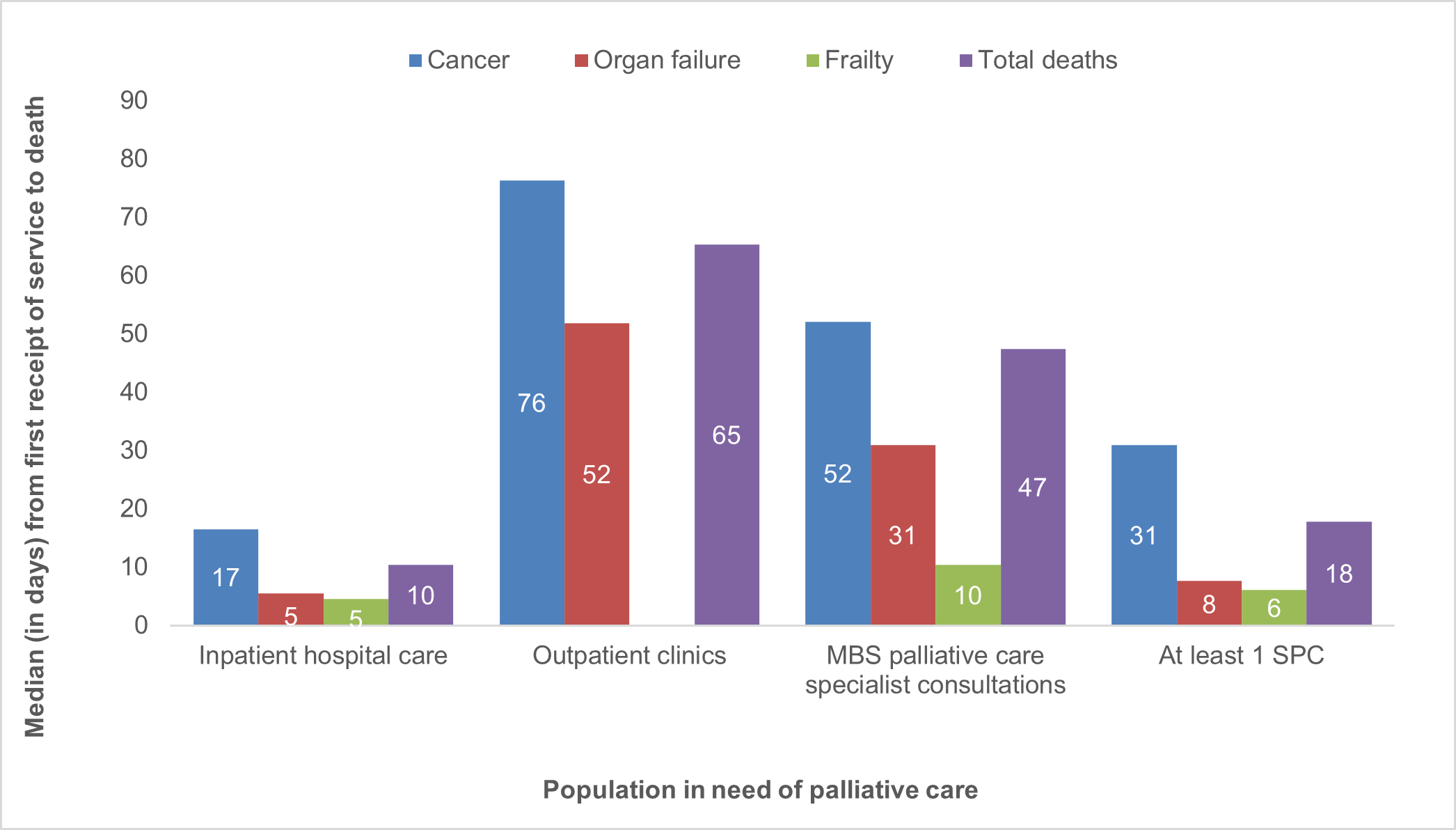
Figure 1b: Median number of days from first receipt of health service to death, by cause of death, for a population in need of palliative care