Introduction
On this page
Although some people die from a single, isolated cause (for example, brain cancer), many people die after long periods of illness while experiencing multiple health conditions, or in a state of frailty and old age.
By looking at all the causes recorded on death certificates we can identify the health conditions that ultimately end a person’s life; those that were responsible for initiating the death; and the conditions that played a significant contributory role in the death. The role of risk factors can be measured to understand the extent they are responsible for a person’s illness or death. The causes most responsible for death in Australia are different depending on which of these ways we look at the causes of death.
From a public health perspective, understanding the different roles played by common causes of death highlights the extent of their involvement in causing death. This can inform different ways to target prevention strategies in addition to what is known about the underlying causes of death.
Where do cause of death statistics come from?
To understand how these different views of cause of death information can be applied, it is useful to get a sense of how the events that cause death play out and are reported (certified) in Australia and translated into data.
All deaths in Australia must be registered with a state or territory Registry of Births, Deaths and Marriages. When a death occurs, a doctor or a coroner must also document what caused the death. This information is recorded on the Medical Certificate of Cause of Death, referred to in this report as the medical death certificate.
For a doctor-certified death, doctors provide their best medical opinion on what caused the persons death, through:
- their knowledge of the deceased person as their patient.
- information in patient medical records.
- information provided by next of kin.
A coroner investigates and certifies deaths which occurred in accidental, unexpected, or unknown circumstances. Coroners investigate the circumstances around the death and determine the cause of death.
The short video below explains how diseases, conditions, and health events are recorded on a death certificate, and how this information is translated for statistical purposes.
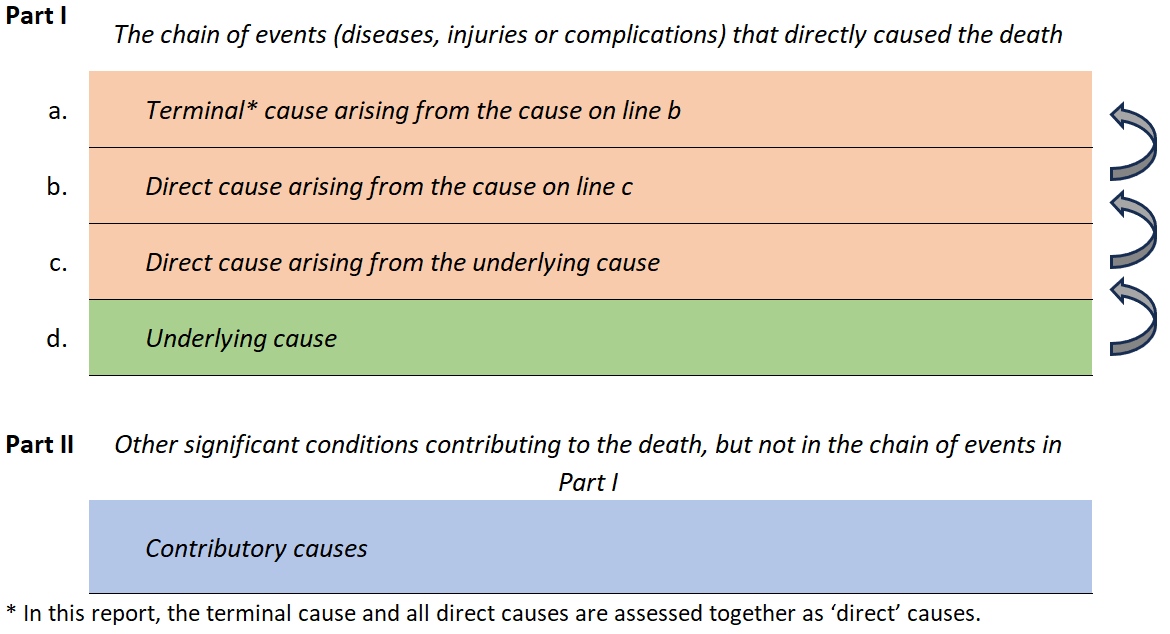
Figure 2.1 shows the standard international format of a medical certificate of cause of death (medical death certificate) and the part and location that is used to record each cause involved in causing the death. Part I is used for describing the underlying cause and the direct causes (the health events arising from the underlying cause) in the chain of events that led to death. In Part II, the certifier describes all other significant medical conditions and other circumstances that contributed to the death (that is, the contributory causes).
Figure 2.1: Cause types assessed in this report based on the international format of the medical certificate of cause of death
International coding standards are applied to the health conditions and circumstances listed on the medical death certificate to identify a single underlying cause, and if present, the direct and contributory causes (see Cause of death terminology).
In Australia, deaths data are compiled and coded by the Australian Bureau of Statistics (ABS). The ABS compiles the annual causes of death data, including doctor- and coroner-certified deaths. Cause of death information is provided to the ABS from the state and territory Registrars of Births, Deaths and Marriages. For coroner-certified deaths, information is also supplied through the National Coronial Information System (NCIS). The information available through the NCIS can provide additional contexts round the death which can enhance coding of the causes of death.
Since 2017 an ABS initiative has improved the availability of information in coroner-certified deaths to include the coding of non-medical psychosocial circumstances associated with a person’s death (ABS 2019).
A more detailed account of the collection and collation of causes of death in Australia is provided by the Australian Bureau of Statistics.
What are the different ways of looking at causes of death?
Traditionally cause of death statistics are generated using only the underlying cause of death, see Deaths in Australia. However, more than one disease or condition can be involved in causing a death. All the information on the death certificate is useful for understanding why the death occurred, and for identifying where interventions could potentially take place to prevent the death occurring.
Conditions which lead directly to death (referred to as ‘direct causes’ in this report) often reflect complications of the underlying cause. These are experienced at the end of life and provide insight into the events experienced directly before death. Terminal conditions are often acute failure of body systems, overwhelming infections, or injuries. Direct causes can also include conditions that are experienced long-term. For example, chronic kidney disease can arise as a complication of diabetes and be present for decades.
People may also have conditions, diseases or contextual factors which didn’t directly lead to or cause death, but their presence contributed to the death. These are referred to as ‘contributory causes’ in this report. Contributory causes can reflect chronic diseases, risk factor-related conditions such as smoking or obesity, and psychosocial factors such as issues with support systems or needs for certain health-related care.
Consideration of all the causes collectively (underlying, direct, and contributory) is referred to as ‘multiple causes of death’ (see Cause of death terminology) and can help understand which types of conditions are most involved in causing death. Using all the causes involved highlights the interplay of multiple diseases or conditions and the role (direct, underlying, or contributory) played by each.
Underlying cause: the condition which initiated the chain of events leading to death. It provides a significant point in the sequence of events where an intervention, if available, could take place to prevent the death from occurring.
Direct causes: the health events that arise from the underlying cause. They can relate to consequences and complications of the underlying cause. Some direct causes reflect the health events experienced at the end of life, or conditions experienced for lengthy periods before death.
Contributory causes: the conditions that significantly contributed to the death but were not in the chain of events leading to death. Typically, these causes relate to prior or co-existing long-term health conditions, and social and other circumstances that were involved in the death. They highlight additional health conditions that could be the focus of prevention strategies, for example, the causes that contribute to chronic disease deaths.
Multiple causes: all the causes involved in causing the death (underlying, direct, and contributory). When assessed in combination these describe the most common conditions involved in causing deaths.
Throughout this report, each of the cause types described above are described in terms of the percentage of deaths they caused as multiple, underlying, direct, or contributory causes. It is important to note that each death can have more than one multiple, direct, or contributory cause.
Why are multiple causes of death important?
Understanding what people die from is vital for informing health programs and policies, not only at a broad population level, but also for age-specific health risks and outcomes. A multiple cause approach to assessing causes of death is necessary to highlight the range of conditions causing death and the extent of their involvement, other than what is known by assessing only the underlying cause. By looking at all the diseases and conditions that contribute to deaths in Australia, a more complete picture of the health status of Australians emerges.
For example, by understanding the conditions or events that cause death in older Australians, preventable causes such as chronic conditions and falls may be better addressed through prevention programs, or improvements in disease and injury management. Collating information for deaths due to suicide, for example, can be used to monitor suicide prevention programs and identify additional areas of support for those who are found to be most at risk of suicide.
Understanding the most common underlying causes of death is important in developing health programs and policies and monitoring population health. However, as death typically results from the interplay between multiple health conditions, focusing solely on the underlying cause can underestimate the impact of other health conditions on a population.
Information on the direct causes of death can lead to improvements in care. It can identify specific prevention strategies such as reducing infection rates in medical settings. Similarly, in deaths due to road traffic accidents, the types of injuries sustained can be better understood. Understanding the types of injuries can inform public health initiatives to target the most severe injuries. An example of this is the measure taken to reduce fatal head injuries by implementing mandatory use of helmets when riding a bicycle (Olivier et al. 2019).
Likewise, information on patterns of the contributory causes of death can identify additional health conditions that could benefit from preventive or intervention strategies, for example, the role of overweight and obesity on premature mortality (Adair and Lopez 2020).
This web report looks at the most common causes of death in Australia using all the information provided on the death certificate. It shows that the answer to the question ‘What do Australians die from?’ can vary depending on what we want to know and the lens through which causes of death are viewed (as underlying, direct, or contributory causes). It identifies frequently occurring causes of death that are less visible when considering only the underlying cause. The report also looks at the psychosocial factors (social determinants) involved in causing deaths that are certified by a coroner, and the impact of leading modifiable risk factors on deaths in Australia.
Adair T and Lopez AD (2020) ‘The role of overweight and obesity in adverse cardiovascular disease mortality trends: an analysis of multiple cause of death data from Australia and the USA’, BMC Medicine, 18: 1–11.
ABS (Australian Bureau of Statistics) (2019) Psychosocial risk factors as they relate to coroner-referred deaths in Australia, ABS, Australian Government, accessed 16 April 2024.
Olivier J, Boufous S and Grzebieta R (2019) ‘The impact of bicycle helmet legislation on cycling fatalities in Australia’, International Journal of Epidemiology, 48(4): 1197–1203, doi:10.1093/ije/dyz003.


