Who has multimorbidity and what are their experiences?
Analysis in this section highlights the personal experiences of people with multimorbidity. Based on self-reported data from the 2017–18 NHS, people with multimorbidity have different characteristics and experiences when compared with those with no self-reported chronic conditions. Comparisons in this section adjust for differences in the age structure of the populations being compared.
The information presented in the following sections relates to people aged 18 or over, due to the scope of the survey population for some of the questions asked. See Box 2 for key considerations for interpreting these characteristics.
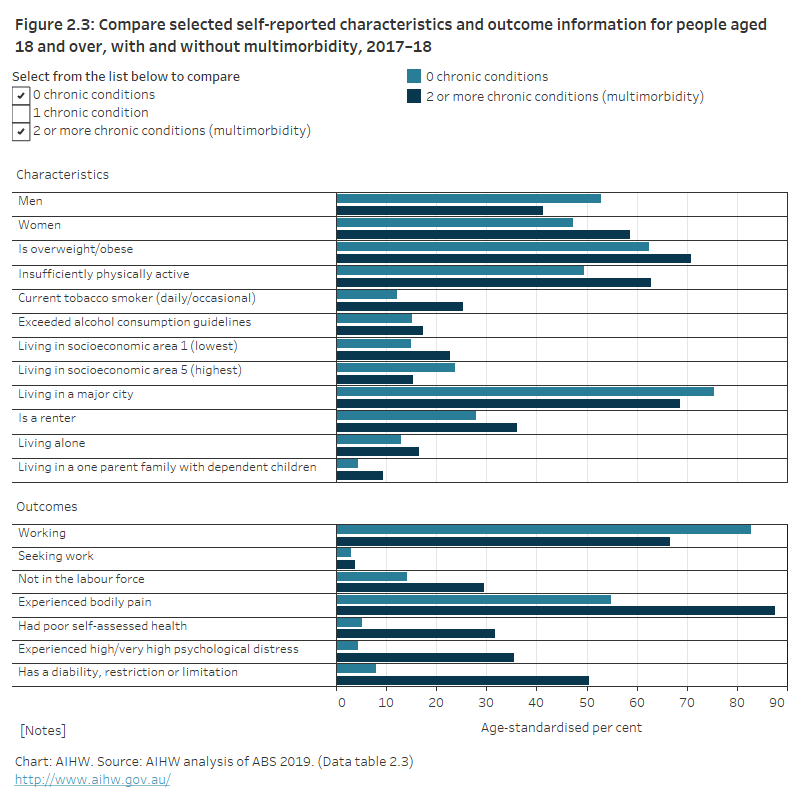
Figure 2.3: Selected self-reported characteristics and outcome information for people aged 18 and over, with and without multimorbidity, 2017–18
This figure shows the proportion of adults with no chronic conditions, 1 chronic condition, or multimorbidity by several self-reported characteristics (including sex, overweight/obesity, current tobacco smoker) and outcomes (including working, bodily pain, disability, restriction or limitation). Compared with people with no chronic conditions, people aged 18 and over with multimorbidity were more likely to be older, women, overweight or obese, not sufficiently active, renting, a current tobacco smoker, living alone or in a one-parent family with dependent children.
Box 2: Key considerations for interpreting common characteristics
It is important to note that while some characteristics, such as age, sex or smoking status, may be more common in people with multimorbidity, it is not possible to say that multimorbidity is caused by these characteristics with the current data. Similarly, it is not possible to say that the characteristics examined are the result of having multimorbidity. For example, while being overweight or obese may be a risk factor for multimorbidity, it could also be the result of a person being limited in the physical activity they can participate in as a result of their multimorbidity. Longitudinal information on when a person developed multimorbidity, and when they became overweight or obese would be needed to understand this, but is not available within the NHS.
Characteristics of people with multimorbidity
Multimorbidity is more common in older age groups (see What is multimorbidity and how common is it?). As a result, the average age of adults with multimorbidity (58 years) is older than those with no chronic conditions (41 years) (ABS 2019).
When comparing people with multimorbidity and those without multimorbidity, it was less common for people with multimorbidity to live in a Major city (69%), compared with people with none of the chronic conditions examined (75% lived in a Major city) (Figure 2.3; Data table 2.3). However, compared with adults with no chronic conditions, those with multimorbidity are more likely to:
- be women (59% of adults with multimorbidity were women, compared with 47% of people with no chronic conditions of the same age)
- be overweight or obese (71% compared with 62%)
- be insufficiently active (63% compared with 50%)
- rent their homes (36% compared with 28%)
- live alone (17% compared with 13%) or in a one-parent family with dependent children (9.3% compared with 4.3%)
- currently smoke tobacco (25% compared with 12%)
- live in areas of highest socioeconomic disadvantage (23% compared with 15%).
The proportion of people who consumed alcohol at levels that put them at a lifetime risk of harm were similar among those with multimorbidity (17%) and those with no chronic conditions (15%).
The National Health and Medical Research Council guidelines for the consumption of alcohol are evidence-based recommendations that aim to reduce the health risks associated with alcohol consumption (NHMRC 2020). The guidelines were updated in 2020 however, estimates here are based on the 2009 guidelines which were current at the time of the survey. Based on the 2009 guidelines, consuming more than 2 standard drinks per day, on average, puts a person at lifetime risk of harm. Information collected from NHS respondents about their alcohol consumption in the week prior to interview is used to estimate the prevalence of lifetime risk of alcohol harm in this analysis. People that consumed alcohol at levels that put them at a lifetime risk of harm may or may not be considered to have an alcohol or drug problem (captured in the ‘mental and behavioural conditions’ group considered in this analysis). See Grouping data for analysis in the Technical notes for details of the definitions and groups used in this analysis.
Experiences of people with multimorbidity
Living with chronic conditions can affect a person’s quality of life and have social and economic effects for the individual (See Box 3). The impact may be even greater for people living with multimorbidity.
Box 3: Multimorbidity in their own words
Below are comments provided by women with multimorbidity in their responses as part of their participation in the Australian Longitudinal Study on Women’s Health. They describe the impact multimorbidity has on multiple aspects of these women’s lives, including physical, emotional, social and financial consequences due to chronic conditions.
“I was forced to retire as a registered nurse because of my limitation. I have had to accept early retirement plus have to pace my activities to be able to control my pain and mobility.”
“I can never feel well enough to do all the things I would like, which can be frustrating and depressing.”
“The frustration of being disabled and not being able to do things that you once could do. Loss of independence and having to ask people for help - extremely difficult.”
“In the last 4 months my physical health has dropped. Where I now need a walker and can no longer do my own shopping.”
“I would normally work full-time but I have been on leave since June last year due to my weakness, tremor, poor eyesight, fatigue etc.”
(Dobson et al. 2020).
People with multimorbidity were less likely to be working than people with no chronic conditions. Two in 3 (67%) people aged 18–64 with multimorbidity were working, compared with 4 in 5 (83%) of people aged 18–64 with no chronic conditions. There was no difference in the proportion of people seeking work (Figure 2.3; Data table 2.3).
Adults with multimorbidity also reported poorer health experiences:
- 88% experienced bodily pain in the previous 4 weeks, compared with 55% of people with no chronic conditions
- 32% had poor self-assessed health, compared with 5.3% of people with no chronic conditions
- 50% had disability, restriction or limitation in everyday activities, compared with 7.9% of people of the same age with no chronic conditions
- 35% had high or very high psychological distress, compared with 4.3% of people with no chronic conditions.
In the 2017–18 NHS, survey participants were asked “In general would you say that your health is excellent, very good, good, fair or poor?” In this analysis, those who rated their health as ‘fair’ or ‘poor’ were grouped under the label poor self-assessed health. See Grouping data for analysis in the Technical notes for details of the definitions and groups used in this analysis.
ABS (Australian Bureau of Statistics) 2019. Microdata: National Health Survey, 2017–18, DataLab. ABS cat. no. 4324.0.55.001. Canberra: ABS. Findings based on Detailed Microdata.
Dobson A, Forder P, Hockey R, Egan N, Cavenagh D, Waller M et al. 2020. The impact of multiple chronic conditions: Findings from the Australian Longitudinal Study on Women’s Health. Report prepared for the Australian Government Department of Health, May 2020.
NHMRC (National Health and Medical Research Council) 2020. Australian guidelines to reduce health risks from drinking alcohol. Canberra: NHMRC.


