Does multimorbidity differ between population groups?
Many health outcomes vary among population groups in Australia. The prevalence of multimorbidity differs by socioeconomic and remoteness areas.
Examining the prevalence of multimorbidity in different population groups can be useful for understanding which groups may be most affected by multimorbidity and therefore might benefit from policies for the prevention or management of multimorbidity.
The findings in this section adjust for differences in the age structure of the populations being compared.
How does multimorbidity vary by socioeconomic area?
The prevalence of multimorbidity was compared across 5 socioeconomic areas, based on the Index of Relative Socio-economic Disadvantage (IRSD). The IRSD reflects the overall, or average, level of disadvantage of the population of an area. It summarises attributes of the population such as low income, low educational attainment, high unemployment and jobs in relatively unskilled occupations, allowing areas to be ranked and compared. See Grouping data for analysis in the Technical notes for more information.
The population living in the areas with the greatest overall level of disadvantage is described as living in the ‘lowest socioeconomic areas’. Generally, people in lower socioeconomic areas are at greater risk of poor health, have higher rates of illness, disability and death, and live shorter lives than people from higher socioeconomic areas (AIHW 2020a; Mackenbach 2015).
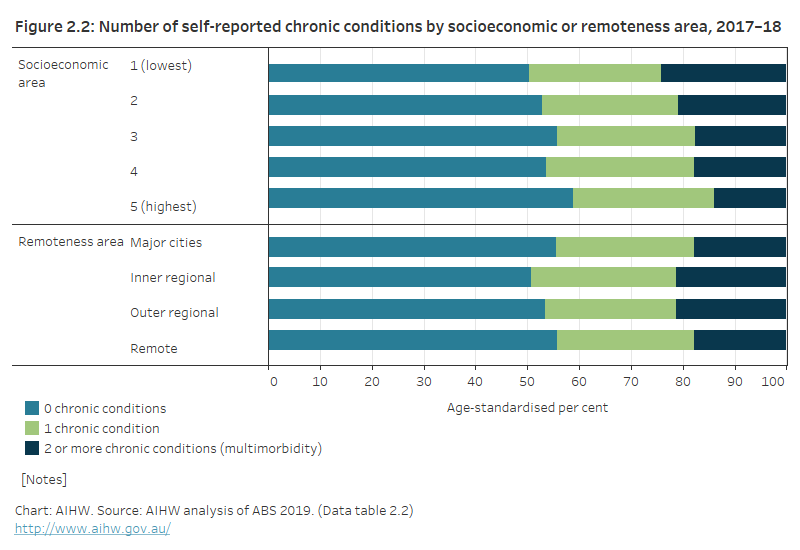
In 2017–18, the prevalence of multimorbidity associated with the 10 self-reported chronic conditions increased with increasing socioeconomic disadvantage, ranging from:
- 1 in 7 (14%) in the highest socioeconomic areas; to
- nearly 1 in 4 (24%) in the lowest socioeconomic areas (Figure 2.2; Data table 2.2).
The proportion of people with 1 chronic condition was similar across socioeconomic areas.
How does multimorbidity vary by remoteness area?
Australians who live in rural and remote areas face unique challenges due to their geographic location (such as accessing health care or specialist services) and often have poorer health outcomes than people living in metropolitan areas. The prevalence of some chronic conditions varies by remoteness area. While people living outside Major cities had higher levels of arthritis, asthma and diabetes in 2017–18, the level of mental and behavioural conditions was higher in Inner regional areas than in Outer regional and remote areas and Major cities. However, the level of other conditions was similar across remoteness areas (AIHW 2020b).
Those living in Major cities were less likely to have multimorbidity than those living in Inner and Outer regional areas. The prevalence of multimorbidity was:
- over 1 in 6 (18%) for people in Major cities and Remote areas
- over 1 in 5 (21%) for people in Inner and Outer regional areas (Figure 2.2; Data table 2.2).
Figure 2.2: Number of self-reported chronic conditions, by socioeconomic or remoteness area, 2017–18
The figure shows the proportion of people with no chronic conditions, 1 chronic condition, or multimorbidity by socioeconomic or remoteness area. The prevalence of multimorbidity increased with increasing socioeconomic disadvantage. The proportion of people in the Major cities with multimorbidity is lower than in Inner and Outer regional areas.
ABS (Australian Bureau of Statistics) 2019. Microdata: National Health Survey, 2017–18, DataLab. ABS cat. no. 4324.0.55.001. Canberra: ABS. Findings based on Detailed Microdata.
AIHW (Australian Institute of Health and Welfare) 2020a. Health across socioeconomic groups. Canberra: AIHW. Viewed 16 November 2020.
AIHW 2020b. Rural and remote health. Canberra: AIHW. Viewed 16 November 2020.
Mackenbach JP 2015. Socioeconomic inequalities in health in high-income countries: the facts and the options. In: Detels R, Gulliford M, Karim QA & Tan CC (eds). Oxford textbook of global public health. Vol. 1. 6th edn. Oxford: Oxford University Press.


