Expenditure on chronic kidney disease
Page highlight:
In 2020–21, $1.9 billion (1.2% of total allocated health expenditure) was attributed to chronic kidney disease.
How much is spent on chronic kidney disease?
In 2020–21, an estimated 1.2% of total allocated expenditure in the Australian health system ($1.9 billion) was attributed to chronic kidney disease (AIHW 2023).
The average health system spending per case of CKD in 2018–19 was $2,326 (males $3,012, females $1,727) (AIHW 2022).
What is expenditure on chronic kidney disease?
This web page provides recent data on health care expenditure on chronic kidney disease (CKD), with details by type of condition, health care service, age group, and sex.
It includes expenditure by the Australian Government; state, territory, and local governments; and the non-government sector (including private health insurance and individual contributions).
These estimates report direct, allocated and recurrent expenditure only. They do not account for the total amount spent on kidney health.
Note: Estimates are not directly comparable to previous disease expenditure estimates due to changes to data and methods. Further information on how the estimates were derived is available from the Disease expenditure in Australia web report.
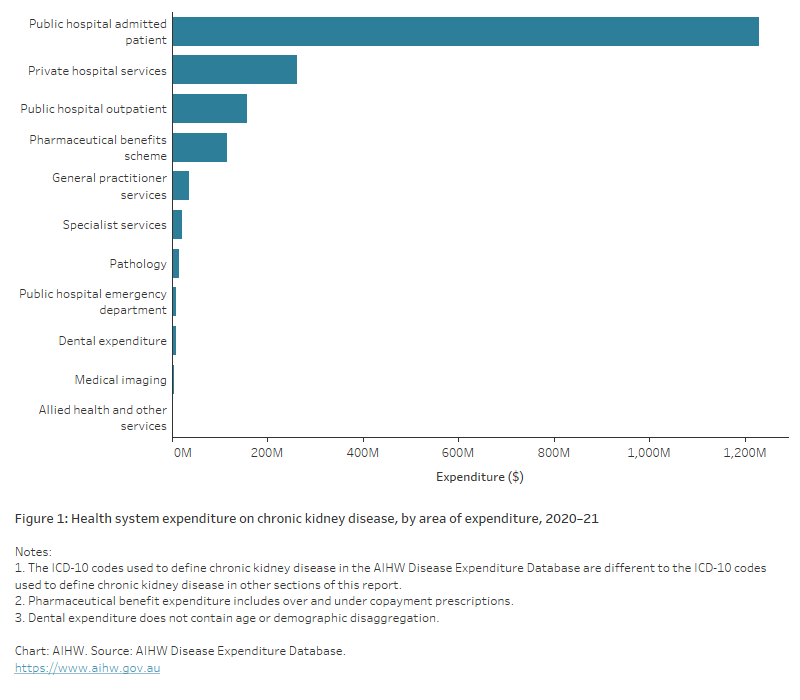
Where is the money spent?
In 2020–21, most allocated CKD expenditure (89% or $1.7 billion) was spent on hospital services. This included expenditure on public hospital admitted patients ($1.2 billion), private hospital services ($261.6 million), public hospital outpatients ($158.1 million) and public hospital emergency departments ($7.8 million).
Another 4% ($76.6 million) related to non-hospital medical services (primary care and referred medical services), comprising general practitioner services ($36.0 million), specialist services ($21.7 million), medical imaging ($3.2 million), pathology ($15.1 million) and allied health and other services ($0.6 million).
A small amount of CKD expenditure (0.4% or $7.6 million) was for dental services.
The remaining 6.3% ($116.2 million) was spent on prescription pharmaceuticals subsidised under the Pharmaceutical Benefits Scheme (PBS) (Figure 1).
Figure 1: Health system expenditure on chronic kidney disease, by area of expenditure, 2020–21
The bar chart shows areas of expenditure on chronic kidney disease in 2020–21. The largest area of expenditure was ‘public hospital admitted patient’ ($1.2 billion), followed by private hospital services, public hospital outpatient services, Pharmaceutical Benefits Scheme services, general practitioner services and specialist services.
Who is the money spent on?
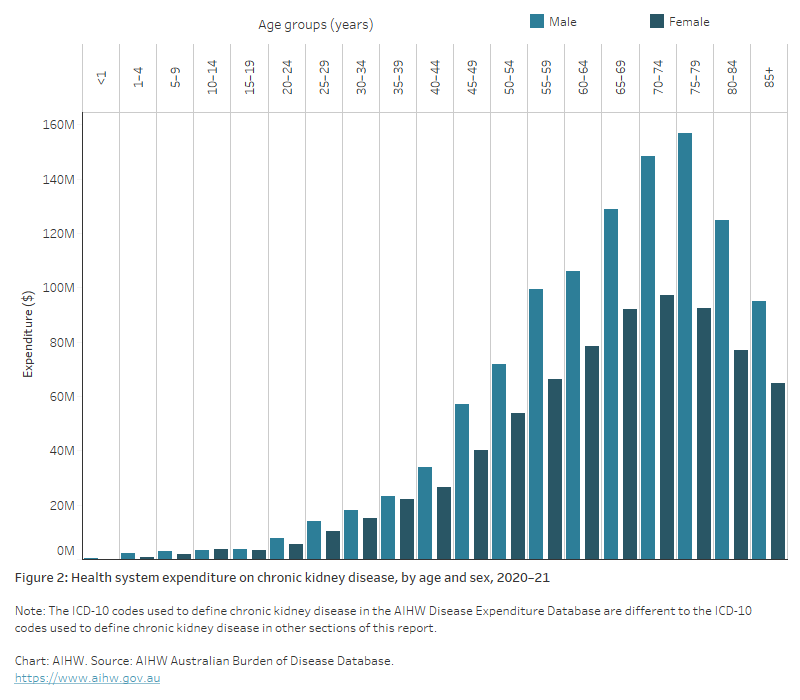
Expenditure on CKD in 2020–21 was low among young people but rose sharply from ages 45–49, to be highest among men aged 75–79 and women aged 70–74 (Figure 2).
Expenditure on CKD was higher among males than females at all ages. From ages 70–74 to age 85 and over, expenditure for men was at least 1.5 times as high as that for women.
Most of this difference related to expenditure on hospital services, where a total of
$993.4 million was spent on males, compared with $662.9 million on females.
Expenditure on non-hospital medical services (primary care and referred medical services) was similar among males and females ($38.4 million and $38.1 million, respectively).
Expenditure on prescription pharmaceuticals under the Pharmaceutical Benefits Scheme was higher among males ($65.9 million) than females ($49.7 million).
Figure 2: Health system expenditure on chronic kidney disease, by age and sex, 2020–21
The bar chart shows expenditure on chronic kidney disease in 2020–21 by age and sex. The overall expense of CKD increased with age to 75–79 years ($250 million). Expenditure was higher for males than females across all age groups.
References
Australian Institute of Health and Welfare (2022) Health system spending per case of disease and for certain risk factors, AIHW, Australian Government, accessed 7 April 2022.
AIHW (2023) Health system spending on disease and injury in Australia, 2020-21, AIHW, Australian Government, accessed 29 November 2023.


