Health risk factors and behaviours
Daily smoking
In 2020–21, 14% of adults with disability were smoking daily, compared with 9.1% of those without disability.
Sugary drinks
In 2020–21, one in 12 (8.3%) adults with disability had sugary drinks daily, compared with 5.6% without disability.
Excessive alcohol consumption
In 2020–21, more than 1 in 3 (36%) men with disability exceeded alcohol consumption guidelines, and 19% of women with disability.
On this page:
Introduction
Health risk factors and behaviours – such as poor diet, physical inactivity, tobacco smoking and excessive alcohol consumption – can have a detrimental effect on a person's health (see Health status for information on the general health of people with disability).
Many health problems experienced by the Australian population, including by people with disability, can be prevented or reduced by decreasing exposure to modifiable risk factors where possible.
People with disability generally have higher rates of some modifiable health risk factors and behaviours than people without disability. But there can be particular challenges for people with disability in modifying some risk factors, for example, where extra assistance is needed to achieve a physically active lifestyle, or where medication increases appetite or affects drinking behaviours.
What are health risk factors and behaviours?
Health risk factors are attributes, characteristics or exposures that increase the likelihood of a person developing a disease or health disorder. They can be behavioural or biomedical.
Behavioural risk factors are those that individuals have the most ability to modify – for example, diet, tobacco smoking and alcohol consumption.
Biomedical risk factors are bodily states that pose direct and specific risks for health – for example, overweight and obesity and high blood pressure. They are often influenced by health behaviours, such as diet and physical activity, but can also be influenced by genetic, environmental, socioeconomic and psychological factors.
Modifying behavioural and biomedical risk factors can reduce a person's risk of developing chronic conditions and result in large health gains by reducing illness and rates of death.
Data note
Data on this page are sourced from the Australian Bureau of Statistics (ABS) National Health Survey (NHS) 2020–21. For more information about the NHS, including the concepts of disability, disability severity, disability groups, and remoteness categories used by the NHS, see Data sources.
The NHS 2020–21 data collection was affected by COVID-19. This impacted on how the data was collected, survey content, and response rates. Because of this, the NHS 2020–21 results are not comparable with previous NHS results. For more information, see Data sources.
The classification of people with disability based on the NHS data in this report is different to the previous versions of People with disability in Australia report. In this report, people with disability or a long-term health condition who have no core activity limitations nor schooling or employment restrictions are included in the group ‘people with disability or long-term health condition’, and are referred to as ‘people with disability’. In the previous versions of the report, they were included in the group ‘people without disability or restrictive long-term health condition’, and were referred to as ‘people without disability’. Therefore, findings in this report are not comparable with the previous versions.
Unless otherwise indicated, all data on this page refer to 2020–21.
Food and nutrition
Food and beverages (our diet) play an important role in overall health and wellbeing. A good diet can:
- contribute to quality of life
- help maintain a healthy body weight
- protect against infection
- reduce the risk of developing chronic conditions.
Health conditions often affected by diet include:
- overweight and obesity
- coronary heart disease
- stroke
- high blood pressure
- some forms of cancer
- type 2 diabetes.
Fruit and vegetable consumption
Fruit and vegetables
Australian dietary guidelines (NHMRC 2013) recommend that adults eat 2 serves of fruit and at least 5 serves of vegetables per day. For children and adolescents, the guidelines recommend 1 to 2 serves of fruit and 2½ to 5½ serves of vegetables per day depending on age and sex. Guidelines are different for pregnant and breastfeeding women.
The guidelines do not apply to people needing special dietary advice for a medical condition, or to the frail elderly. As such, they should be treated with caution for some people with disability (for example, those with medical conditions requiring a special diet).
In the ABS NHS, adequacy of intake (consumption) is based on whether a respondent's reported usual daily fruit or vegetable intake meets or exceeds the NHMRC recommendation. It is collected for people aged 2 and over. The results presented in this report and accompanying supplementary data tables are in most cases limited to adults aged 18 and over.
Many people, including those with disability, do not eat enough fruit and vegetables for optimum health and wellbeing. Based on self-reported data, in 2020–21 around half (55%) of adults aged 18 and over with disability were eating less than the recommended serves of fruit and less than the recommended serves of vegetables each day, and were slightly more likely than people without disability (51%) to not meet the guidelines (Figure RISK.1).
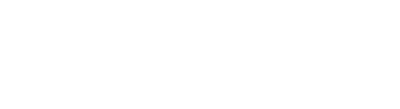
Figure RISK.1: Consumption of fruit and vegetables, by disability status, sex and age group, 2020–21
The chart shows adults with and without disability are both less likely to meet guidelines for vegetable consumption than for fruit consumption.

Notes:
- Restricted to people aged 18 and over living in households.
- Based on 2013 National Health and Medical Research Council (NHMRC) Australian Dietary Guidelines.
- The categories ‘Eat enough fruit’ and ‘Eat enough vegetables’ also include people who eat enough of both fruit and vegetables.
- Data have been randomly adjusted to avoid identifying individual people.
Source data tables: Data tables – Health risk factors and behaviours. View data tables
Consumption of fruit and vegetables by people with disability varies between males and females, and with age (Figure RISK.1):
- Males aged 18 and over with disability (62%) are more likely than females (49%) to not eat enough fruit or vegetables each day.
- The inadequate intake of fruit and vegetables is highest for the 18–64 age group at 60%, compared with 45% for people aged 65 and over with disability and 42% for children (aged 2–17) with disability (ABS 2022). This is consistent with patterns for the overall population (see AIHW food and nutrition for more information).
More than half of adults aged 18 and over across most disability groups do not eat enough fruit or vegetables:
- 54% of those with sensory or physical disability do not meet either fruit or vegetable guidelines
- 57% of those with intellectual disability
- 63% of those with psychosocial disability
- 48% of those with head injury, stroke or acquired brain injury (ABS 2022).
Sugar-sweetened and diet drinks
Australian dietary guidelines recommend limiting intake of discretionary items, such as sugar-sweetened drinks and diet drinks, as they tend to have little nutritional value. Limiting intake may help manage some health conditions.
What are sugar-sweetened and diet drinks?
The ABS NHS includes information on the usual daily consumption, in the previous week, of selected sugar-sweetened drinks and diet drinks.
Sugar-sweetened drinks include soft drinks, cordials, sports drinks or caffeinated energy drinks. This may include soft drinks in ready-to-drink alcoholic beverages but excludes fruit juice, flavoured milk, sugar-free drinks, coffee and hot tea, and alcoholic beverages (that is, beer and wine).
Diet drinks have artificial sweeteners in place of sugar. These include diet soft drinks, cordials, sports drinks or caffeinated energy drinks. This may also include diet soft drinks in ready-to-drink alcoholic beverages but excludes non-diet drinks, fruit juice, flavoured milk, water or flavoured water, coffee and tea flavoured with sugar replacements (for example, the brand Equal), and alcoholic beverages (that is, beer and wine).
Adults with disability are about 1.5 times as likely to consume sugar-sweetened drinks and diet drinks daily as those without disability (based on self-reported data):
- 8.3% of adults aged 18 and over with disability consume sugar-sweetened drinks daily, compared with 5.6% of adults without disability
- 9.2% of adults aged 18 and over with disability consume diet drinks each day, compared with 6.1% of those without disability (Figure RISK.2).
The consumption of sugar-sweetened drinks varies by sex, age group, and disability group:
- Males aged 18 and over with disability are more than twice as likely (12%) to consume sugar-sweetened drinks daily as females (5.2%).
- Adults with disability aged 18–64 are more than twice as likely (10%) to consume sugar-sweetened drinks daily as those aged 65 and over (4.3%).
- 12% of adults with psychosocial disability consume sugar-sweetened drinks daily, compared with 5.9% of those with sensory disability (ABS 2022).
The consumption of diet drinks varies by disability severity and sex:
- Adults with severe or profound disability are more likely (17%) to consume diet drinks daily than those with other disability status (8.2%)
- 11% of males aged 18 and over with disability consume diet drinks daily compared with 7.5% of females (ABS 2022).
Figure RISK.2: Daily consumption of sugar-sweetened and diet drinks, by disability status, sex, and age group, 2020–21
The chart shows that a higher proportion of men with disability consume sugar-sweetened drinks daily (12%) than men without disability (7.2%).

Notes:
* Relative standard error of 25–50% and should be used with caution.
- Restricted to people aged 18 and over living in households.
- Sugar-sweetened drinks include soft drinks, cordials, sports drinks or caffeinated energy drinks. May include soft drinks in ready to drink alcoholic beverages.
- Diet drinks have artificial sweeteners in place of sugar. These include diet soft drinks, cordials, sports drinks or caffeinated energy drinks. May include diet soft drinks in ready to drink alcoholic beverages.
- Data have been randomly adjusted to avoid identifying individual people.
Source data tables: Data tables – Health risk factors and behaviours. View data tables
Physical activity
Getting enough exercise is an important factor in maintaining good physical and mental health and wellbeing.
What is physical activity?
Physical activity includes just about any movement resulting in energy expenditure, such as:
- taking part in a deliberate exercise or sport, like playing tennis or swimming
- muscle strengthening activity, like weight training
- incidental movement, like mowing the lawn
- work-related activity, like lifting.
Physical activity and exercise guidelines for all Australians (Department of Health and Aged Care, 2021) define sufficient physical activity for adults as:
- adults aged 18–64: 150 to 300 minutes of moderate physical activity or 75 to 150 minutes of vigorous physical activity (or an equivalent combination) over 5 or more days per week, and muscle strengthening activities on at least two days per week
- adults aged 65 and over: at least 30 minutes of physical activity per day.
These guidelines are aimed at everyone irrespective of cultural background, gender, or ability. However, they may not be appropriate for people with some forms of disability and may not fully take into account that, for some groups of people with disability, such as those with mobility issues, getting enough exercise can be particularly challenging. Physical activity for people with disability or chronic or acute medical conditions is still important, but the type and amount should be appropriate to a person's ability and based on advice from health-care practitioners. The availability of inclusive gyms and exercise spaces can play an important role for some people with disability to participate in physical activity.
In the ABS NHS, people aged 15 and over are asked to report the intensity, duration and number of sessions spent on physical activity during the week before the survey (including at work). The results presented in this report and accompanying supplementary data tables are in most cases limited to adults aged 18 and over.
For more information on physical activity, see AIHW physical activity.
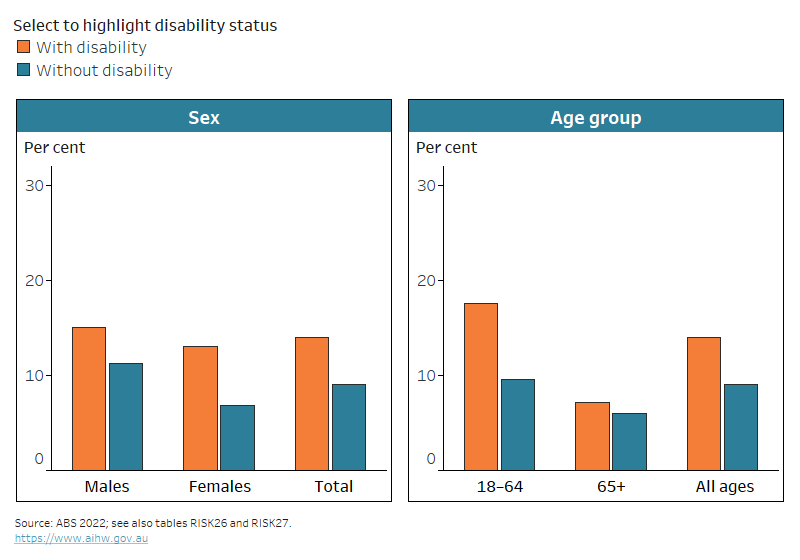
Many people, including those with disability, are not getting enough exercise. Based on self-reported data, nearly three-quarters (74%) of adults aged 18 and over with disability in 2020–21 did not do enough physical activity (including at work) for their age; this was similar for those without disability (71%).
Among adults (aged 18 and over) with disability, physical activity was lower for:
- adults with severe or profound disability (of whom 14% had enough physical activity), compared with adults with other disability status (27%)
- adults with psychosocial (16%) or intellectual (18%) disability, compared with adults with physical restriction (23%), or sensory or speech disability (30%)
- women with disability (23%) compared with men (29%) (Figure RISK.3; ABS 2022). This is consistent with patterns for the overall population.
Figure RISK.3: Proportions of people getting enough physical activity, by disability status and severity, sex, and age group, 2020–21
The chart shows adults aged 18–64 with disability are less likely to meet the physical activity guidelines (19%) than those without disability (26%).
Notes:
* Relative standard error of 25–50% and should be used with caution.
- Restricted to people aged 18 and over living in households.
- Based on Australia's Physical Activity and Sedentary Behaviour Guidelines 2014–15.
- Data have been randomly adjusted to avoid identifying individual people.
Source data tables: Data tables – Health risk factors and behaviours. View data tables
People aged 65 and over, both with and without disability, are more likely to meet physical activity guidelines than people aged 18–64, most likely due to differences in the guidelines for the two age groups:
- 37% of people with disability aged 65 and over (47% without disability) had enough physical activity, compared with 19% of people with disability aged 18–64 (26% of those without disability) (Figure RISK.3).
Among adults aged 18–64 with disability, physical activity declines with age:
- 33% of adults with disability aged 18–24 get enough physical activity
- 23% of adults with disability aged 25–44
- 14% of those aged 45–64 (ABS 2022).
Tobacco smoking
Tobacco smoking is an important cause of preventable ill health and death in Australia. It is a leading risk factor for the development of many chronic conditions and premature death.
Health conditions often affected by tobacco smoking include many types of cancer, respiratory disease and heart disease.
What is tobacco smoking?
Tobacco smoking is the smoking of tobacco products, including packet cigarettes, roll-your-own cigarettes, cigars and pipes.
In the ABS NHS, people aged 15 and over are asked:
- if they currently smoke
- if they were ex-smokers or had never smoked
- about the frequency and quantity of their smoking.
Because daily smoking presents the greatest health risk, the results presented on this page relate to people who were daily smokers at the time of the survey. The results presented in this report and accompanying supplementary data tables are limited to adults aged 18 and over.
For more information, see AIHW smoking and e-cigarettes.
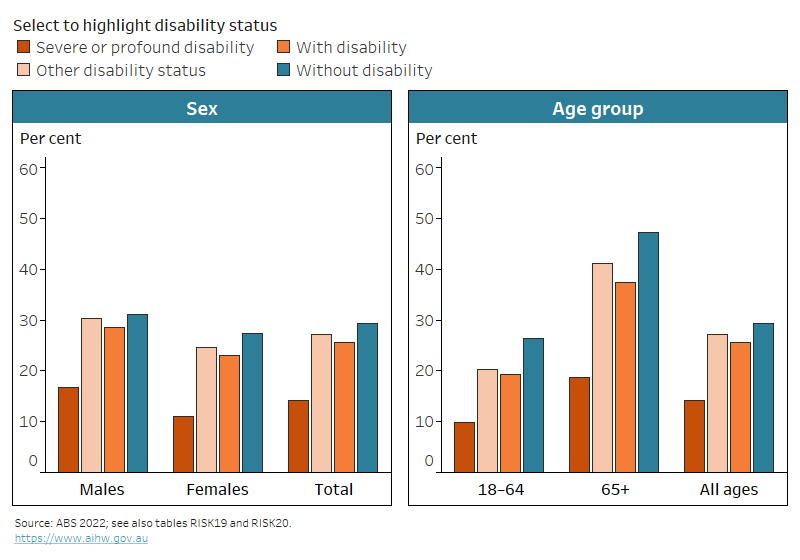
About 1 in 7 (14%) adults aged 18 and over with disability smoke daily (based on self‑reported data). They are more likely to do so than people without disability (9.1%). Younger adults (aged 18–64) with disability are almost twice as likely (18%) to smoke daily as those without disability (9.5%). This is not the case for older adults (aged 65 and over). The proportion of older adults with disability who are daily smokers (7.2%) is similar to those without disability (6.0%) (Figure RISK.4).
Males aged 18 and over with disability are about as likely (15%) to smoke daily as their female counterparts (13%) (Figure RISK.3), but females aged 18 and over with disability are more likely to have never smoked (60%) than males (41%) (ABS 2022).
Adults (aged 18 and over) with psychosocial disability are more likely (24%) to smoke daily than those with sensory disability (11%) or physical disability (15%) (ABS 2022).
Figure RISK.4: Daily tobacco smoking, by disability status, sex and age group, 2020–21
The chart shows that women with disability are more likely to smoke daily (13%) than women without disability (6.8%).
Notes:
- Restricted to people aged 18 and over living in households.
- Current daily smokers are those who reported at the time of interview that they regularly smoked one or more cigarettes, cigars or pipes per day.
- Data have been randomly adjusted to avoid identifying individual people.
Source data tables: Data tables – Health risk factors and behaviours. View data tables
E-cigarette use and vaping
E-cigarettes and vaping devices do not produce the tar produced by conventional cigarettes which is the main cause of lung cancer. However, many scientists are concerned that using e-cigarettes could increase risk of lung disease, heart disease and cancer. Since October 2021, e-cigarettes that contain nicotine can only be accessed through a prescription in Australia (Department of Health and Aged Care 2023). Given these changes have come after the data period reported in this section, any impacts of this change will not be apparent until subsequent data collections.
What are e-cigarettes and vaping devices?
An e-cigarette is a device that heats a liquid to produce vapours that users inhale. This may contain nicotine and other toxic chemicals. E-cigarette use is also commonly referred to as vaping. In this report, e-cigarette use includes the use of vaping devices and/or e-cigarettes.
The ABS NHS 2020–21 introduced new questions on the use of e-cigarettes and vaping. People aged 15 and over were asked:
- if they currently use an e-cigarette or vaping device
- if they had ever used an e-cigarette or vaping device
- about the frequency and quantity of their e-cigarette use or vaping.
The results presented in this report and accompanying supplementary data tables are limited to adults aged 18 and over.
Based on self-reported data from the ABS NHS 2020–21, the use of e-cigarettes and vaping devices is similar for adults aged 18 and over with and without disability:
- 1.8% of adults aged 18 and over with disability are daily e-cigarette users, as are 1.3% of those without disability
- 7.6% of adults with disability have used an e-cigarette in the past or use it less often than daily, and 8.0% of those without disability
- 91% or adults with and without disability have never used an e-cigarette (ABS 2022).
Alcohol consumption
Harmful levels of alcohol consumption are a major health issue and are associated with increased risk of chronic conditions and injury.
What is risky alcohol consumption?
Alcohol consumption refers to the consumption of drinks containing ethanol, commonly referred to as alcohol. The quantity, frequency or regularity with which alcohol is drunk provides a measure of the level of alcohol consumption.
Australian guidelines to reduce health risks from drinking alcohol (NHMRC 2020) provide advice on reducing the risk of harm from alcohol-related disease or injury. Based on the guideline for adults, the ABS NHS 2020–21 defines excessive alcohol consumption as:
- consuming more than 10 standard drinks of alcohol per week, and/or
- consuming 5 or more standard drinks of alcohol in one day at least monthly over the last 12 months.
In 2020–21, the NHS collected information about alcohol consumption for people aged 15 and over. It should be noted that the above definition of risky alcohol consumption is for people aged 18 and over, and that the current guidelines state that children and young people under 18 years of age should not be drinking alcohol. The results presented in this report and accompanying supplementary data tables are limited to adults aged 18 and over.
For more information, see AIHW alcohol.
Based on self-reported data, more than 1 in 4 (27%) adults (aged 18 and over) with disability exceed the recommended alcohol consumption guideline, similar to those without disability (25%) (Figure RISK.5).
Figure RISK.5: Whether exceeded recommended alcohol consumption guidelines, by disability status and severity, sex and age group, 2020–21
24% of men with severe/profound disability exceeded the alcohol consumption guideline, 37% with other disability status and 32% without disability.
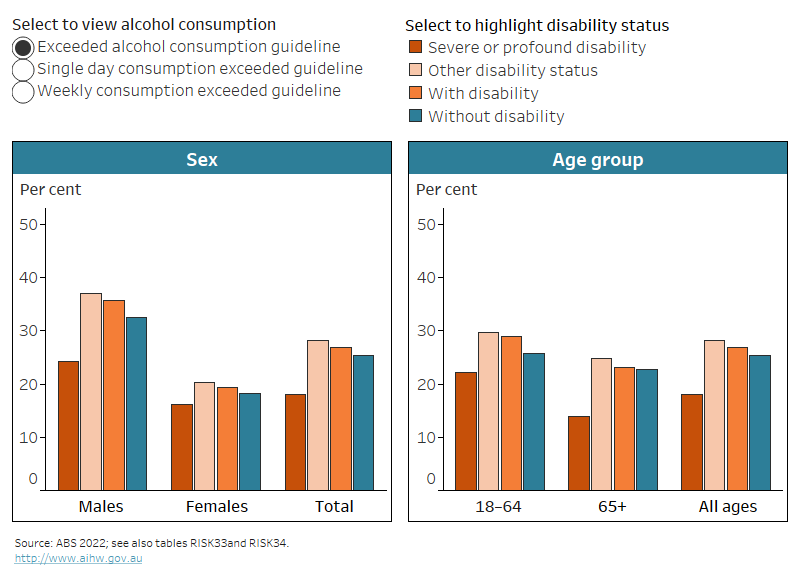
Notes:
* Relative standard error of 25–50% and should be used with caution.
- Restricted to people aged 18 and over living in households.
- Based on the alcohol consumption guideline for adults from the National Health and Medical Research Council (NHMRC) released in 2020.
- Exceeding the weekly consumption guideline is defined as consuming more than 10 standard drinks in the past week.
- Exceeding the single day consumption guideline is defined as consuming 5 or more standard drinks in one day at least monthly over the past year.
- Exceeding the alcohol consumption guideline is defined as exceeding the single day and/or weekly consumption guideline.
- Data have been randomly adjusted to avoid identifying individual people.
Source data tables: Data tables – Health risk factors and behaviours. View data tables
Although overall and single-day excessive alcohol consumption levels were similar for adults with and without disability, adults with disability were more likely to exceed the weekly alcohol consumption guideline than those without disability:
- 23% of adults with disability drink more than 10 standard drinks per week, compared with 19% of adults without disability
- 17% of both adults with and without disability drink 5 or more standard drinks in one day at least monthly (ABS 2022).
The alcohol consumption of people with disability varies by sex, age group and disability severity.
Males aged 18 and over with disability are far more likely than their female counterparts to drink at risky levels:
- 36% of males exceed the alcohol consumption guideline compared with 19% of females (Figure RISK.5)
- 31% consume more than 10 standard drinks of alcohol per week, compared with 15%
- 24% consume 5 or more standard drinks of alcohol on a single occasion each month, compared with 11% (ABS 2022).
There is similar variation of alcohol consumption patterns by sex among people without disability (Figure RISK.5; ABS 2022).
Younger adults (aged 18–64) with disability are more likely (29%) to exceed the alcohol consumption guideline than older adults (aged 65 and over) (23%) (Figure RISK.5). Younger adults with disability are:
- twice as likely (21%) to consume 5 or more standard drinks in a single occasion at least monthly as older adults with disability (9.7%).
- about as likely to consume more than 10 standard drinks per week as older adults with disability (24% compared with 21%) (ABS 2022).
There is similar variation of alcohol consumption patterns by age group among people without disability (Figure RISK.5; ABS 2022).
Adults with severe or profound disability are less likely (18%) to exceed the alcohol consumption guideline than those with other disability status (28%) and are also less likely to consume more than 10 standard drinks of alcohol per week (15% compared with 24%) (Figure RISK.5; ABS 2022).
Where can I find out more?
- Data tables for this report.
- Health risk factors and behaviours for the general Australian population – Behaviours & risk factors.
- ABS key statistics and information about Dietary behaviour, Physical activity, Smoking and vaping, and Alcohol consumption.
- Dietary guidelines – National Health and Medical Research Council (NHMRC).
- Physical activity and exercise guidelines – Department of Health and Aged Care (DHAC).
- Guidelines to reduce health risks from drinking alcohol – National Health and Medical Research Council (NHMRC).
ABS (Australian Bureau of Statistics) (2018) ABS sources of disability information, 2012–2016, ABS cat. no. 4431.0.55.002, ABS, accessed 4 August 2021.
ABS (2022) Microdata and TableBuilder: National Health Survey, ABS, AIHW analysis of detailed microdata in DataLab, accessed 4 May 2023.
DHAC (Department of Health and Aged Care) (2021) Physical activity and exercise guidelines for all Australians, DHAC, Australian Government, accessed 1 June 2023.
DHAC (2023) About vaping and e-cigarettes, DHAC, Australian Government, accessed 1 June 2023.
NHMRC (National Health and Medical Research Council) (2013) Australian Dietary Guidelines, NHMRC, accessed 4 August 2021.
NHMRC (2020) Australian guidelines to reduce health risks from drinking alcohol, NHMRC, accessed 2 June 2023.